Better Sleep Through Healthy Habits and Understanding Your Mind
Why Sleep Matters
Good sleep restores your body and brain, supporting mood, focus, metabolism, and resilience. Americans are getting less sleep than ever, and sleep deprivation creates an inflammatory state in the body. An often overlooked fact of life is that most medical and mental health problems can be improved by improving disordered sleep.
Sleep is incredibly important. You should prioritize it, and you should protect it!
Many people who struggle with sleep are not experiencing a primary sleep disorder, but are suffering the consequences of poor sleep hygiene or a sleep disturbance related to stress, anxiety, trauma, or other psychiatric issues. Treating the root cause—whether through therapy, lifestyle changes, or safe use of medications—can greatly improve sleep.
The goal is to break the cycle of worry, frustration, and exhaustion by creating a plan that restores confidence in your ability to sleep and conditions where good sleep happens.
Consider that you may have sleep apnea or restless leg syndrome if you snore, gasp, or feel exhausted despite long sleep. Check sleephealthscreen.com for a quick online assessment.
Resetting Your Sleep Cycle
Use your brain’s natural mechanisms to reset your internal clock.
If your sleep schedule drifts late or feels “off,” you may need to reset your circadian rhythm:
- Melatonin: Take a small dose (0.5–3 mg) in the early evening (2–4 hours before bedtime), not right before bed. This signals your body that night is approaching. Don’t overdo it with melatonin—buy 1mg tablets and break them in half—find the right dose and dial it in.
- Evenings: limit your exposure to blue light at night because it suppresses the brain’s release of melatonin.
- Mornings: expose yourself to bright white or blue-enriched light (sunlight or a 10,000 lux lamp) within 30 minutes of waking. This helps reinforce a healthy wake–sleep rhythm.
- Consistency: Keep regular wake times, even on weekends.
For guidance, try the CBT-i Coach app developed by the U.S. Department of Veterans Affairs: https://mobile.va.gov/app/cbt-i-coach
The Science Behind Short-Term Sleep Deprivation
Allowing mild sleep deprivation for a day can improve long-term insomnia outcomes. Sometimes we might do a big reset in order to straighten your sleep out.
When we try to “fix” sleep by sleeping in, napping, or using excess caffeine, we interrupt these systems. Instead, a little short-term sleep deprivation can help your body reset. Allow adenosine to build up, avoid naps, and trust your body’s ability to recalibrate.
Healthy Sleep Hygiene: First Aid for Insomnia
Sleep hygiene means building the habits and environment that support sleep. It’s not about perfection—it’s about reducing interference so your natural sleep system can work.
1. Build a Strong Sleep Routine
- Go to bed and wake up at roughly the same time every day.
- Sleep only as long as you need to feel refreshed—too much time in bed can worsen sleep quality.
- If you can’t sleep after ~20 minutes, get out of bed and do something calm (read, stretch, listen to soft music). Return to bed when sleepy.
2. Make Your Bedroom a Sanctuary
- Keep your room cool (65–68°F), quiet, and dark.
- Use white noise, earplugs, or heavy curtains if you live near noise.
- Avoid electronics, work, or worry in bed—reserve your bed for sleep and sex.
- Replace worn-out mattresses or pillows.
3. Support Sleep With Daily Habits
- Exercise regularly (morning or late afternoon are best). Exercise before bed may delay sleep onset slightly but still improves sleep depth.
- Avoid caffeine after 2 p.m. Caffeine blocks adenosine—the chemical that makes you sleepy.
- Avoid alcohol at night. It may make you drowsy but leads to fragmented, shallow sleep and early awakenings.
- Skip nicotine before bed—it stimulates the nervous system.
- Eat dinner at least 3 hours before bedtime and avoid heavy, spicy, or acidic foods late at night.
4. Manage Light and Screens
- Use blue light filters on devices in the evening.
- Dim indoor lighting and wear blue-light blocking glasses in the evening.
- Stop using phones or computers at least 30–60 minutes before bed.
- Charge your phone outside the bedroom.
5. Keep a Sleep Diary
Track your bedtime, wake time, caffeine/alcohol intake, exercise, and mood. Patterns often reveal what’s helping or hurting your sleep.
6. Rethink Substances
- Caffeine: Even morning coffee can affect sensitive sleepers.
- Alcohol: Makes sleep fragmented; avoid it near bedtime.
- Cannabis: Can reduce REM sleep and worsen rebound insomnia when stopped.
- Tobacco: Nicotine delays sleep onset and causes lighter sleep.
7. Address Underlying Causes
Sleep can be affected by mental health conditions, medical issues, or medications:
- Anxiety and rumination: Try mindfulness, journaling, or CBT-based tools.
- Depression: Combine sleep regularity with daytime activity and sunlight.
- Trauma: Nightmares and fear of sleep are common; therapy and medications like prazosin may help.
- Medication-induced insomnia: Talk to your prescriber about adjusting timing or alternatives.
8. Trust Your Body
Trying too hard to sleep backfires. Don’t force it. Only go to bed when truly tired, and if you can’t fall asleep, leave the bed until you are. The unconscious brain runs the “sleep gears”—trying to manually control them creates insomnia. When in doubt, get up, move to a dimly lit room, and return when drowsy.
Small Steps, Big Results
Changing sleep patterns can feel hard, especially when anxiety builds around bedtime. Focus on small, realistic changes:
- Adjust bedtime gradually (15 minutes earlier per night).
- Try one new sleep hygiene habit per week.
- Celebrate progress rather than focusing on perfection.
Remember: the goal is better rest, not instant sleep. Over time, consistency and calm confidence will restore your natural rhythm.
When Medication Is Appropriate
Some people benefit from short-term or adjunctive medication.
You might be thinking that you should ask for an Ambien® prescription, but I’m going to be real with you—Ambien® sucks. Better options include:
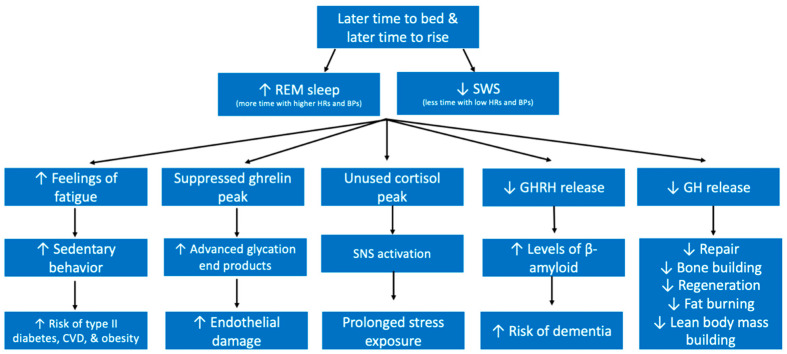
- Trazodone: Helps maintain sleep and reduces nightmares. Trazodone also improves sleep architecture by increasing slow wave sleep (SWS).
- Gabapentin: Useful for anxiety, trauma-related insomnia, and substance use reduction—it also improves SWS.
- Hydroxyzine: Not habit-forming, can aid anxiety and sleep.
- Doxepin (low dose): Effective for sleep maintenance; available in liquid form, also not habit-forming.
Avoid chronic or high-dose use of sedative-hypnotics (benzodiazepines, “Z-drugs” like Ambien® or Lunesta®). Medications should complement—not replace—behavioral strategies.
If we need to prescribe you a controlled substance, it will probably be an orexin antagonist like Dayvigo® or Belsomra®.
Helpful Resources
- CBT-i Coach App: https://mobile.va.gov/app/cbt-i-coach
- SleepHealthScreen: https://sleephealthscreen.com
- National Sleep Foundation: https://www.thensf.org
- CDC Sleep Guidelines: https://www.cdc.gov/sleep/about_sleep/how_much_sleep.html
Key Takeaway: You can train your brain and body to sleep better by combining structure, light exposure and exercise during the day, calm routines at night, and healthy behaviors. Medications and therapy can support you—but the foundation of great sleep is built by your daily habits.
Understanding the stages of sleep
During a healthy night of rest, your brain cycles through several stages roughly every 90 minutes.
Each stage plays a unique role in restoring the body and mind:
- Stage 1 – Light Sleep: This is the gentle transition from being awake to asleep. Muscles relax, breathing slows, and you can wake easily. It helps your body wind down.
- Stage 2 – Deeper Light Sleep: Your body temperature and heart rate drop further. The brain produces short bursts of activity called sleep spindles, which are believed to support learning and memory.
- Stage 3 – Deep Sleep: Also called slow-wave sleep, this is the most restorative phase. Tissue growth and repair occur, immune function strengthens, and the brain clears out waste. Waking during this stage often causes grogginess.
- REM Sleep – Dream Sleep: Brain activity increases, vivid dreams occur, and the mind processes emotions and consolidates memories. REM sleep supports mood, creativity, and problem-solving.

A full night of good-quality sleep includes several of these cycles. When stress, alcohol, caffeine, or inconsistent habits disrupt them, the body misses key opportunities for healing and mental refreshment.
Using technology to improve sleep
Neurofeedback devices and wearable sleep trackers can help you finely dial in your sleep. There are two that I generally recommend.
Using neurofeedback headbands (like the Muse S Athena) and sleep-tracking wearables (like the Ultrahuman Ring) can help improve sleep by giving you real-time insight into your brain and body, so you can make targeted adjustments instead of guessing what’s wrong. Here’s how each contributes and how they can work together:
🧠 Muse S Athena – Real-Time Neurofeedback for Relaxation & Sleep Onset
What it does:
- Uses EEG-like sensors to read your brain’s electrical activity and translate it into audio feedback (like calm sounds or guiding voices).
- Helps you learn when your mind is calm, focused, or distracted by giving you immediate cues, training your brain to enter a more relaxed state before bed.
- Offers guided meditation, breath pacing, and “sleep journeys” designed to reduce pre-sleep rumination and anxiety—two major causes of insomnia.
- Tracks brain-wave patterns during sleep, showing time spent in light, deep, and REM stages.
How it helps:
- Regular use strengthens your ability to self-regulate stress and transition into sleep more smoothly.
- Acts as “biofeedback training” for the mind, teaching relaxation skills that lower nighttime cortisol and help you fall asleep faster.
- By identifying nights of excess beta-wave (alert) activity, it can reveal when stress or stimulants are preventing deep rest.
💍 Ultrahuman Ring – Sleep and Recovery Tracking
What it does:
- Measures heart-rate variability (HRV), resting heart rate, skin temperature, oxygen levels, and movement to assess sleep stages and recovery quality.
- Provides detailed reports on sleep efficiency, latency, disturbances, and circadian rhythm consistency.
- Integrates with daily activity, glucose, and nutrition data to show how exercise, caffeine, or late meals affect sleep.
How it helps:
- Gives objective feedback on how lifestyle factors (screen time, alcohol, meal timing, workouts) influence your sleep architecture.
- Detects subtle signs of overtraining or stress (via HRV drops) so you can adjust before sleep quality suffers.
- Encourages consistency through “readiness scores” and personalized nudges—turning good sleep into a measurable daily goal.
🌙 Using Them Together
- Muse S trains your brain to relax and fall asleep more easily.
- Ultrahuman Ring monitors how your body responds overnight.
- Together, they create a feedback loop: you can see how your pre-bed mindfulness session or breathing exercise (guided by Muse) directly affects your sleep efficiency and deep-sleep duration (measured by the Ring).
🧩 Clinical Insight
Both tools bridge the gap between psychology and physiology. Instead of relying only on subjective impressions (“I think I slept badly”), you gain quantitative feedback that helps personalize interventions—whether that’s adjusting bedtime, limiting caffeine, or adding evening relaxation exercises. Over time, this approach builds self-awareness, routine consistency, and improved restorative sleep.
