What it means to take a holistic approach to the treatment of depression
Depression isn’t one-size-fits-all. At Happy Healthy New York, we combine the latest science with a whole-person approach to care. Depression can have many causes, so a full workup means doing some digging. Some patients come to HHNY after trying standard antidepressants without success. What sets us apart is our commitment to biological investigation, testing, measurable outcomes, and integrative interventions that target both the mind and body.
Many patients achieve remission with medication alone, though combination treatment with psychotherapy is often more effective, especially for severe depression. The medications can make you feel well enough so you can make the changes in your life that will bring you out of depression—getting physically active, socializing, sleeping right, using light as medicine, and working with a therapist.
The most important parts of your journey out of depression happen in between our visits, in your daily life. Happy Healthy New York recommends therapy for everyone with depression, and we can refer you to a therapist, but the scope of what we do together will be on identifying the causes of your depression and treating symptoms with lifestyle, medications, and advanced interventions. The goal is remission and living a happy, healthy life with great physical and mental health.
Step 1: Understanding the Biology — Ruling Out Organic Causes
Testing and screening
Depression can sometimes arise from underlying biological imbalances. Before we label anyone as having “treatment-resistant” depression, we perform a comprehensive medical workup to identify or rule out reversible causes.
We commonly assess for:
- Vitamin D deficiency: Low levels are linked to low mood, especially in winter months.
- Inflammation (hs-CRP): Elevated C-reactive protein can signal inflammatory depression. There’s evidence to suggest that some people have inflammation-related depression and may respond to certain treatments.
- Hormonal imbalances: Thyroid, testosterone, and estrogen levels can all impact mood, focus, and energy.
- Nutrient deficiencies: Folate, B12, and Omega-3 levels influence neurotransmitter synthesis and brain health.
- Routine screening for substance use, sleep apnea, anemia, and infectious diseases (e.g., HIV, syphilis, Lyme disease) is recommended, as these medical conditions and medication effects can mimic or exacerbate depressive symptoms and may be missed without systematic evaluation.
These lab tests help us determine whether a patient’s depression may have a physiological component. When we identify these issues early, we can often correct them and see meaningful improvement before medication changes are even needed.
We also use validated clinical scales to track your symptoms objectively over time. That means we can measure progress, not just hope for it.
Step 2: Building the Foundation — Lifestyle and Nutrition
One of the best ways to not be depressed is to stop acting like a depressed person would act.
Once we’ve ruled out biological causes, we move to foundational lifestyle strategies. These habits form the backbone of brain health and emotional stability.
Behavioral Activation:
Structured, meaningful activity is one of the most powerful antidepressants we have. We help patients build daily routines that include social engagement, physical movement, and exposure to natural light.
Mediterranean Diet:
We emphasize whole foods—rich in vegetables, legumes, protein, and olive oil. This pattern reduces inflammation, supports the microbiome, and stabilizes energy levels.
Targeted Supplementation:
- Omega-3 fatty acids (EPA-rich): Improve neuronal flexibility and communication.
- Vitamin D: Corrects deficiencies and supports healthy immune-brain signaling.
- Magnesium and methylfolate: Aid in neurotransmitter production and calm nervous system reactivity.
- Probiotics and fiber: Strengthen the gut-brain connection, which influences mood regulation.
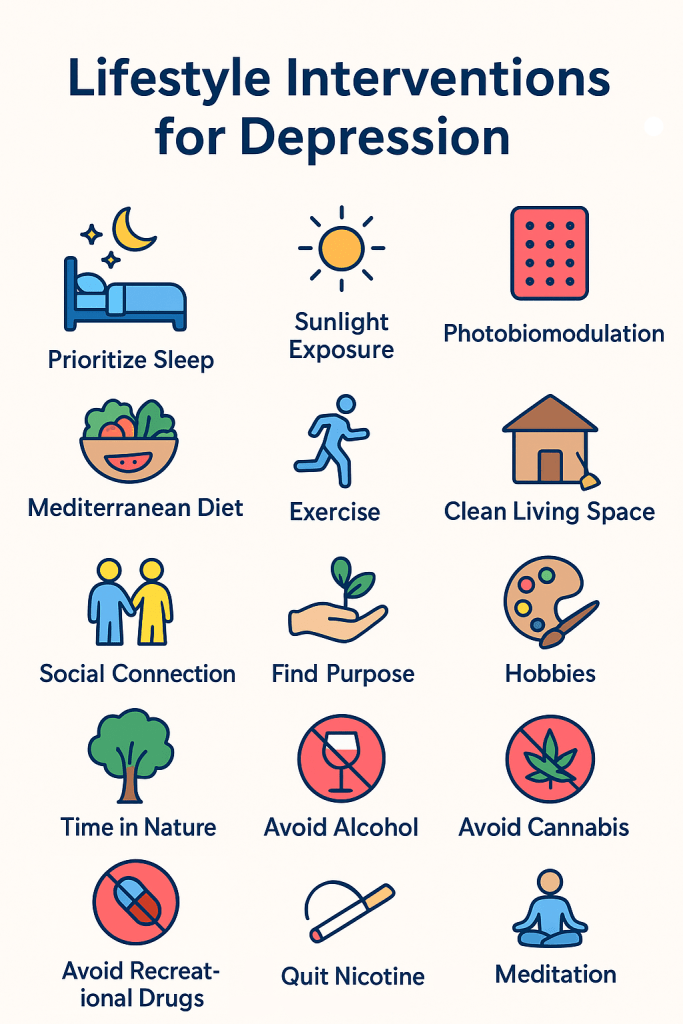
Lifestyle interventions:
After reading these 6 steps, you’ll find 15 interventions that you can start implementing this week to improve your symptoms and take control of your life. By taking small steps we can build the framework for a happier healthier life.
The meds support neuroplasticity—the brain’s ability to grow, adapt, and heal. The interventions are the places where we want that growth to take place.
Step 3: Harnessing Light and Energy — Photobiomodulation (PBM)
PBM enhances mitochondrial energy production in brain cells, increasing cerebral blood flow, and promoting neuroplasticity through increased brain-derived neurotrophic factor (BDNF).
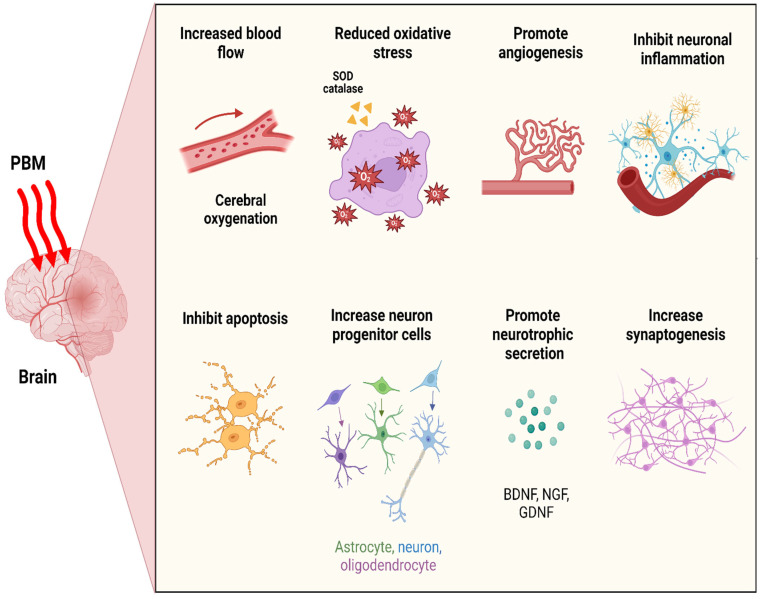
We integrate red and near-infrared light therapy (photobiomodulation) to activate mitochondrial energy production and improve mood at the cellular level.
Photobiomodulation (PBM) can be a powerful tool in treating depression. Red and near-infrared wavelengths enhance neuroplasticity by increasing brain-derived neurotrophic factor (BDNF) levels, promoting synaptogenesis, and improving cognitive function in both healthy and pathological states. PBM also supports healthy sleep patterns, with systematic reviews and randomized controlled trials demonstrating improvements in sleep quality and efficiency, likely mediated by enhanced cerebral mitochondrial activity, blood flow, and glymphatic clearance during sleep.
Light can be delivered transcranially (through the scalp) or systemically (to other body areas), with recent evidence suggesting systemic approaches may produce larger effects.
We also use blue light photobiomodulation and bright-light therapy, and find this especially effective for patients whose depression follows seasonal patterns or circadian rhythm disturbances. Just 20–30 minutes of morning light exposure can lift energy and stabilize sleep cycles. The VA guidelines recommend photobiomodulation of this variety as a first line intervention regardless of whether or not the depression is seasonal, and we are here for that big time.
Step 4: Evidence-Based Medications — Tailored to the Individual
Medication management with pharmacotherapy
If lifestyle and biological interventions aren’t enough, we turn to conventional pharmacologic treatments—but with precision.
Every patient’s situation is different, so we select medications based on their specific symptoms, values, and past responses. We also use lab and genetic insights to minimize side effects and maximize benefit.
The typical HHNY approach includes:
- SSRIs, bupropion, mirtazapine, and other medications that lumped into the category of “antidepressants.” We’ll talk about which, if any, might be right for you and what you can expect.
- Using pharmacology to help you sleep better if that’s a problem area for you. Sleep has a bidirectional relationship with depression.
- Lithium augmentation can help some people. Buspirone can help others.
- T3 (liothyronine) to enhance antidepressant response when thyroid function is low
- Nutritional and hormonal augmentation when deficiencies are found. Did you know that testosterone and estrogen are protective against depression?
Throughout our time together, we continue tracking outcomes with validated rating scales to make data-driven adjustments and track your progess.
Step 5: Advanced Interventions — Ketamine, Esketamine, and TMS
Interventional approaches when the basics aren’t enough.
The HHNY approach is not satisfied by modest improvements in depression. You wouldn’t want a modest improvement in cancer or heart disease, right? So why would you want to stay moderately depressed?
Ketamine & Esketamine (Spravato):
These medications act on the NMDA receptor, rapidly boosting neuroplasticity and restoring connections in brain regions affected by depression. Many patients experience relief within hours to days—especially those with long-standing, treatment-resistant depression or suicidal thoughts.
Transcranial Magnetic Stimulation (TMS):
A completely non-invasive therapy that uses focused magnetic fields to stimulate underactive areas of the brain. TMS is FDA-approved, well-tolerated, and effective in helping patients who haven’t responded to medication alone.
Step 6: Long-Term Maintenance and Growth
Keeping you well
Depression recovery isn’t just about symptom relief—it’s about resilience. We work with patients to maintain improvements through:
- Periodic re-testing of key labs (vitamin D, CRP, thyroid, hormones)
- Ongoing therapy (CBT, ACT, or trauma-focused approaches)
- Optional TMS, ketamine, or esketamine maintenance treatments.
- Continued emphasis on lifestyle, community, and purpose
The Happy Healthy New York Approach
Our mission is to combine science, compassion, and measurable outcomes. Depression is complex, but healing doesn’t have to be mysterious. By combining biological testing, lifestyle science, and state-of-the-art interventions, we can help you understand why you feel the way you do—and chart a path toward recovery that’s personalized, evidence-based, and empowering. Essential to this approach is a therapeutic alliance where we are working towards the same goal.
Next, let’s cover fifteen lifestyle changes you can start this week to improve your depression and move you closer to the life you want to live.
Implementing Lifestyle Interventions for Depression: Evidence-Based Strategies
Depression is a complex condition, but research shows that certain lifestyle changes can make a huge impact in managing symptoms and improving overall well-being.
Medication is helpful for many people, but it’s rarely sufficient on its own. Nonpharmacologic interventions fill out the rest of the picture, and when these are used alongside antidepressants, people tend to do much better.
Here’s a guide to fifteen practical, evidence-backed interventions you can start today.
Regardless of whether we are using therapy or medications to treat your depression, making lifestyle changes are an absolutely critical part of resolving depression. Funny as it may seem, one of the best treatments for depression is to stop acting like a depressed person and go do things a depressed person wouldn’t do—that isn’t fake it ’til you make it, that’s called behavioral activation.
1. Prioritize Sleep
Establishing a regular sleep routine, creating a calming environment, and limiting caffeine and alcohol late in the day can help regulate your mood and energy. Poor sleep is closely linked to depression, and improving sleep hygiene is a proven strategy for symptom relief.
Evidence:
Dysfunctional sleep and depression bidirectionally impact each other, and improving one often improves the other. The impact that sleep has on mental health is difficult to overstate. If your sleep is disordered, this is your top priority lifestyle intervention.
2. Increase Exposure to Sunlight
Getting more natural sunlight helps regulate your circadian rhythm and boosts vitamin D, both of which are linked to mood regulation.
Evidence:
This SR/meta-analysis from the Journal of Happiness Studies discusses the broad impacts of light on wellbeing. A fascinating study focusing on operating room nurses (who get no sunlight at work) found they exhibit poorer mental health than other populations, and nurses’ mental health was better with longer sunlight exposure time. Did you know that a 75-year-old needs 3 times as much light in order to trigger the same response as a 45-year-old? Circadian abnormalities have been observed as prodromal indicators or Alzheimer’s & Parkinson’s disease.
3. Photobiomodulation
Photobiomodulation (light therapy, particulary NIR + red light) is emerging as a promising intervention for depression.
Evidence:
This 2025 meta-analysis found the effect size reported for photobiomodulation to be very powerful (PBM overall, SMD ≈ –0.55) and actually much stronger than the average effect sizes usually seen for SSRIs (≈ 0.36) or psychotherapy (≈ 0.25 vs placebo, ~0.02 difference vs SSRIs). What’s important to note is that there is much more data for SSRIs and psychotherapy than PBM, and I think that a multi-faceted approach is very often the best strategy. Read more about PBM here—HHNY patients know I really get excited about this.
4. Eat a Mediterranean-Style Diet
A diet rich in omega-3s, low in added sugars, and based on whole foods (like the Mediterranean diet) is associated with lower rates of depression.
Evidence:
A 2019 meta-analysis found that adherence to a Mediterranean diet and increased omega-3 intake is effective in the treatment of depression both alone and when combined with antidepressants.
5. Exercise Regularly
Physical activity is one of the most effective non-pharmacological treatments for depression.
6. Clean Your Living Space
A tidy, organized environment can help reduce stress and improve mood.
Evidence:
This 2018 meta-analysis reviews the relationship between living environment and depressed mood. Did you know that that stressful situations cause fish, birds, and mammals to engage in cleaning behaviors which serve functions for defense and relaxationl? This study explores physiological evidence for the attenuation of stress-related effects by cleaning in humans and animals.
7. Stay Connected
Social isolation can worsen depression. Connecting with friends, family, or even pets can lift your mood.
Evidence:
A longitudinal analysis found that social support and reduced loneliness are strongly associated with lower depression severity.
8. Find Purpose
Engaging in meaningful activities or volunteering can provide a sense of purpose and buffer against depression.
Evidence:
A 2013 systematic review found that volunteering and purposeful activities are associated with lower rates of depression and improved well-being.
9. Enjoy Relaxing Hobbies
Spending time on hobbies you enjoy can reduce stress and improve mood.
Evidence:
A 2021 review article in Lancet Psychiatry discusses the literature that shows engagement in leisure activities, including hobbies, is associated with lower depression risk.
10. Spend Time in Nature
Nature exposure is linked to better mental health and reduced depressive symptoms.
Evidence:
A 2019 systematic review found that spending time in nature significantly reduces symptoms of depression and anxiety.
11. Avoid Alcohol for Coping
Using alcohol to cope can worsen depression, disrupt sleep, and cause problems in your life.
Evidence:
A meta-analysis in the Journal of Substance Abuse Treatment found that 60.5% of people with above-average levels of depressive symptoms show above-average levels of alcohol use, and that women with alcohol use disorder tend to be more depressed than men. People who drink a lot of alcohol have alcohol-related problems, like fighting with their partners and failing to meet obligations. Even a small dose of alcohol interferes with sleep, and sleep is one of the most important modifiable factors in depression.
12. Avoid Recreational Drugs
Recreational drugs can disrupt brain chemistry and make depression harder to treat.
Evidence:
A 2020 meta-analysis explores substance use’s is association with increased risk and severity of depressive disorders
13. Avoid Cannabis
Cannabis use is associated with higher levels of anxiety and depression.
14. Quit Nicotine
Smoking is associated with increased risk of depression, and quitting can improve mental health.
Evidence:
A 2021 umbrella review found that smoking cessation is associated with reduced depression and improved mental health outcomes.
15. Start meditating
Mindfulness-based practices, including meditation, have demonstrated modest efficacy in reducing depressive symptoms. This is free to do, relaxing, and effective.
Evidence:
This 2023 systematic review found that mindfulness practices reduced depression and anxiety scores with a similar effect size to pharmacotherapy.
