
If you’re struggling with low mood, anxiety, or motivation, we are likely to have a brief discussion on how certain systems in the brain work. On this page we’ll take a deeper dive to discuss the neurologic and metabolic aspects of our brains and how this affects our mood, motivation, cognition, and mental & physical health. The topics covered here include holistic wellbeing, nonpharmacologic interventions, neurotransmitters, endorphins, and hormones. While this won’t be a fully comprehensive guide, it will cover the most important topics about the things going on in your head. This page can serve as a reference for patients who are looking to gain deeper understanding into biological processes influencing mental health and some of the ways we can tweak biology in our favor. A lot of the science here will be also applicable to other pages on the site like addiction, depression, photobiomodulation, and medical weight loss.
Though this page will mostly cover technical science topics, you’ll notice that simple lifestyle interventions consistently improve the complicated neurometabolic pathways discussed on this page. Holistic methods first! Grab the high-impact low-hanging fruit before trying to tweak the other stuff.
Holistic wellbeing & interventions for a healthy brain
Sleeping, Eating, Socializing, and Exercising
Sleep is critical for neurotransmitter balance, hormonal regulation, and neuroplasticity. You can improve your sleep with good sleep hygiene. High quality sleep is a function of the following components: schedule, substances (alcohol, caffeine, nicotine), avoiding naps, suitable bedtime activities, light exposure, diet, and exercise.
| Goal: 7–9 hours per night. Interventions: – Maintain a consistent sleep/wake schedule. – Avoid stimulants (caffeine, nicotine) and alcohol before bed. – Use light exposure strategically (bright light in the morning, dim lights in the evening). – Practice a calming bedtime routine; avoid screens in the last hour. |
Diet and nutrition influences inflammation, neurotransmission, and neurotrophic factors. Eating a Mediterranean diet can improve mental health by reducing inflammation, supporting the gut-brain axis, and providing neuroprotective effects that lower the risk and severity of depression, anxiety, and cognitive decline.
| Mediterranean diet: High in fruits, vegetables, whole grains, olive oil, fish, nuts; moderate wine if appropriate. Neuroprotective nutrients: – Omega-3 fatty acids: Improve BDNF, neuroplasticity, and mood. – Polyphenols (berries, grapes, vegetables, nuts): Reduce oxidative stress and neuroinflammation. – Prebiotic fiber: Supports gut microbiota that produce short-chain fatty acids and modulate serotonin metabolism. |
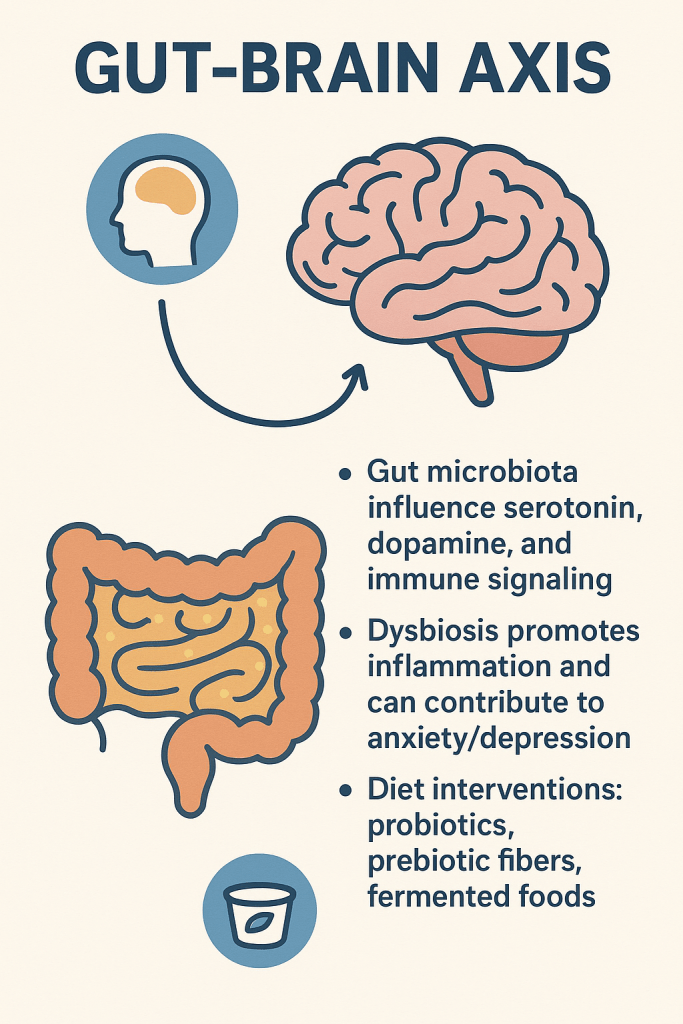
Dysbiosis (disruption to your normal gut microbiome) promotes inflammation and can contribute to anxiety/depression. Support your microbiome with fermented foods and prebiotic/probiotics.
Social connectivity directly influences mood-regulating neurochemistry (oxytocin, dopamine, endorphins). Be kind to other people. Join group activities and volunteer with organizations. Review these CDC tips for ways to increase your social connectivity.
| – Regular interactions with family, friends, or community groups. – Volunteer work or joining interest-based clubs |
Exercise improves mental health by releasing endorphins, dopeamine, and BDNF—reducing stress, enhancing mood, improving sleep, and boosting self-esteem. Regular physical activity is associated with lower levels of anxiety and depression, and it can be an effective part of treatment for various mental health conditions.
| Aerobic: brisk walking, cycling, swimming, dancing Resistance: weightlifting, Pilates, functional strength training Mind–Body: Yoga, Tai Chi, meditation-based movement |
Stress Management
Chronic stress impairs neurotransmitter function, BDNF, and HPA axis regulation.
| Interventions: Mindfulness, meditation, deep breathing (Box Breathing), cognitive restructuring, journaling, time in nature. |
Emerging Lifestyle Domains
| Cold/Heat exposure: Sauna and cold immersion increase BDNF, norepinephrine, and endorphins. Cognitive training: Learning new skills strengthens cortical connectivity. Chronotherapy: Morning light exposure helps entrain circadian rhythms, supporting melatonin and cortisol balance. |

The WHO-5 Wellbeing Index was adapted into the HERO Wellness Scale, which assesses holistic mental wellness from a positive psychology perspective. HERO covers four aspects of mental health that matter in our daily wellbeing.
Cutivate positive mind-states in order to improve your mental wellbeing.
| HERO Category | Specific Interventions |
|---|---|
| Happiness | + Practice daily gratitude journaling + Engage in enjoyable activities and hobbies + Foster positive relationships and social connections + Volunteer or perform acts of kindness + Spend time in nature or green spaces |
| Enthusiasm | + Set meaningful short & long-term goals + Start the day with a motivating morning routine + Pursue new interests or learning opportunities + Celebrate small achievements + Surround yourself with positive, energetic people |
| Resilience | + Practice mindfulness or meditation + Develop problem-solving and coping skills + Practice breathing techniques like Box Breathing + Maintain a regular exercise routine + Seek support from peers or mentors during challenges + Reflect on past successes in overcoming adversity |
| Optimism | + Reframe negative thoughts into positive ones + Visualize positive outcomes + Limit exposure to negative news or influences + Read or listen to inspiring stories + Practice self-compassion and positive self-talk |
Ok, now one more time let’s just run through this stuff; it’s important and worth repeating:
| Category | Subcategory | Suggested Interventions |
|---|---|---|
| Exercise | Aerobic Exercises | Brisk walking, jogging, cycling, swimming, dancing, group fitness classes |
| Resistance Training | Weightlifting, bodyweight exercises, resistance bands, Pilates, functional strength training | |
| Nutrition | Meeting Protein Requirements | Lean meats (occasionally if at all), fish, eggs, dairy, legumes, tofu, nuts, and seeds in daily meals. |
| Meeting Fiber Requirements | Eat whole grains, fruits, vegetables, legumes, nuts, and seeds. | |
| Limiting Processed Foods | Reduce intake of packaged snacks, sugary drinks, fast food, and processed meats. | |
| Mediterranean Diet Lifestyle | Emphasize vegetables, fruits, whole grains, olive oil, fish, nuts, and moderate wine consumption but no other alcohol. | |
| Sleep | Sleep Hygiene | Maintain a cool, dark, quiet bedroom; avoid screens before bed; establish a bedtime routine. |
| Consistent Schedule | Go to bed and wake up at the same time every day, including weekends. | |
| Getting Enough Sleep | Aim for 7–9 hours of sleep per night in a dark, cool room. | |
| Social Connections | Spend Time with Loved Ones | Schedule regular family meals, phone calls, or visits with friends and relatives. |
| Seek Opportunities to Socialize | Join clubs, volunteer, attend community events, participate in group activities. | |
| HERO mindset | Happiness Enthusiasm Resilience Optimism | – Engage in enjoyable activities and hobbies – Set goals and learn things – Develop coping skills – Reframe negative thoughts into positives |
| Limit Harmful Substances | Quit Smoking | Use cessation aids, behavioral therapy, or support groups. |
| Limit Drinking | Set limits on alcohol intake, choose alcohol-free days, opt for non-alcoholic alternatives | |
| Don’t Do Drugs | Avoid recreational drug use, seek support if needed |
Neurotransmitters
These are complicated, but I’ve created a table that discusses (in broad strokes) their function and ways they can be tweaked to optimize function.
| Neurotransmitter | Functions | Lifestyle Interventions to Optimize Function | Medications Affecting Neurotransmitter |
| Dopamine | Reward, motivation, motor control, mood regulation | Regular exercise, adequate sleep, stress reduction, protein-rich diet | Dopamine agonists (pramipexole), L-DOPA, antipsychotics (block D2), MAO-B inhibitors, bupropion, stimulants |
| Serotonin | Mood, appetite, sleep, pain perception, cognition | Sunlight exposure, exercise, meditation, tryptophan-rich foods | SSRIs, SNRIs, 5-HT receptor agonists/antagonists |
| Norepinephrine | Attention, arousal, stress response, mood | Physical activity, stress management, adequate sleep | SNRIs, norepinephrine reuptake inhibitors, bupropion, stimulants (methylphenidate, amphetamines) |
| Epinephrine | Fight-or-flight response, increases heart rate and blood flow | Stress management, regular exercise | Adrenergic agonists (epinephrine, albuterol), beta-blockers (antagonists) |
| Histamine | Wakefulness, immune response, gastric acid secretion | Allergen avoidance, healthy sleep hygiene, balanced diet | Antihistamines (H1 and H2 blockers), some antidepressants are histamine antagonists (like mirtazapine) which can help sleep |
| Acetylcholine | Memory, learning, muscle activation, autonomic regulation | Cognitive stimulation, physical activity, healthy fats in diet | Acetylcholinesterase inhibitors (donepezil), anticholinergics (atropine) |
| GABA | Main inhibitory neurotransmitter, reduces neuronal excitability | Relaxation techniques, meditation, regular exercise | Benzodiazepines, barbiturates, GABA analogs (gabapentin) |
| Glutamate | Main excitatory neurotransmitter, learning, memory | Balanced diet, avoid excitotoxins, stress reduction | NMDA antagonists (memantine, ketamine), anticonvulsants |
| Glycine | Inhibitory neurotransmitter in spinal cord and brainstem | Adequate protein intake, physical therapy | Glycine receptor agonists/antagonists (rare, experimental) |
| Substance P | Pain transmission, inflammation | Pain management, stress reduction | NK1 receptor antagonists (aprepitant) |
| Neuropeptide Y | Appetite regulation, stress response, anxiety modulation | Stress management, regular exercise | Experimental NPY receptor modulators |
| Endocannabinoids | Mood, appetite, pain, stress | Exercise, diet, sleep | Experimental cannabinoid modulators |
| Endorphins | Natural pain relief, mood elevation | Aerobic exercise, laughter, social bonding | Opioid receptor agonists (morphine, oxycodone), naloxone & naltrexone (antagonists) |
Endorphins
β-endorphin, enkephalins, and dynorphins are the most important endorphins, acting via opioid receptors to mediate analgesia, mood, and stress responses. Their function can be optimized through regular physical activity and positive social interactions. Certain pharmacologic agents such as antidepressants and NSAIDs, which may enhance endogenous opioid activity.
| Endorphin Type | Main Receptor Target(s) | Primary Actions | CNS/PNS Role |
| β-endorphin | μ-opioid receptor | Pain relief, euphoria, reward | Both central and peripheral |
| Met/Leu-enkephalin | δ- and μ-opioid | Pain relief, mood modulation | Both central and peripheral |
| Dynorphins | κ-opioid receptor | Pain relief, dysphoria, stress | Both central and peripheral |
β-endorphin is the most prominent and well-studied endorphin. It is produced primarily in the pituitary gland and hypothalamus and acts as a potent agonist at the μ-opioid receptor, leading to analgesia (pain relief), euphoria, and modulation of the stress response. Enkephalins and dynorphins are also important, with enkephalins primarily targeting δ-opioid receptors and dynorphins acting on κ-opioid receptors.
Mechanisms of Action
- β-endorphin binds to opioid receptors (primarily μ-opioid) in the CNS and PNS, inhibiting the release of neurotransmitters involved in pain transmission and stress, and modulating the hypothalamic-pituitary-adrenal (HPA) axis.
- It exerts analgesic effects at the spinal, supraspinal, and peripheral levels.
- β-endorphin also influences the secretion of pituitary hormones (e.g., ACTH, prolactin, growth hormone) and reduces catecholamine levels in the brain, particularly dopamine, which is involved in reward and mood regulation.
Role in Mental Health
- Mood and Euphoria: β-endorphin is associated with feelings of well-being and euphoria, and is implicated in the reward and reinforcement pathways of the brain.
- Stress and Anxiety: Endorphins modulate the stress response and may buffer against anxiety and depressive symptoms by regulating the HPA axis and neurotransmitter release.
- Addiction and Reward: β-endorphin contributes to the reinforcing effects of certain drugs and behaviors, playing a role in addiction and substance use disorders.
Lifestyle Interventions to Optimize Endorphins:
- Physical Exercise: Aerobic and endurance exercise (e.g., running, cycling) robustly increases endorphin release, contributing to the “runner’s high” and improved mood.
- Social Interaction and Laughter: Positive social engagement and laughter stimulate endorphin release.
- Meditation and Mindfulness: Practices such as yoga and meditation can enhance endogenous opioid activity.
- Music and Art: Enjoyable sensory experiences, including music and creative activities, may also boost endorphin levels.
Pharmacologic Interventions:
- Antidepressants: Certain antidepressants like SSRIs & SNRIs may indirectly modulate endorphin pathways improving mood and pain, though this is not their primary mechanism. Activation of serotonin 5-HT1A receptors by these agents has been shown to increase β-endorphin release. This effect may contribute to their mood-elevating and anxiolytic properties.
- NSAIDs (e.g., ibuprofen, naproxen): Some evidence suggests NSAIDs may enhance analgesia (pain relief) by increasing β-endorphin activity, though the exact mechanisms remain under investigation.
- Opioid Agonists: Exogenous opioids (e.g., morphine, oxycodone) mimic endorphin action but carry significant risk for dependence and are not used to optimize endogenous function—in fact, opioid drugs can actually distort and hypersensitize the endogenous nociceptive system, making chronic pain worse. Chronic opioid use also causes dysphoria/depression and suppresses sex hormones leading to impotence in men, menstrual irregularities in women, and feelings of fatigue.
Hormones
There are too many hormones to list tem all here, but the most important hormones for mental and metabolic health include cortisol, insulin, thyroid hormones, sex steroids (estrogen, testosterone), melatonin, and leptin. Below is a table summarizing their normal serum levels, physiologic pathways, and lifestyle interventions to optimize their function.
| Hormone | Normal Serum Level (Adult) | Physiologic Pathway & Role | Lifestyle Interventions to Optimize Function |
| Oxytocin | 1-10 pg/mL | As a hormone, oxytocin is released into blood from the pituitary gland. It plays a role in various reproductive processes. As a neurotransmitter, oxytocin is released within the brain. It’s involved in social behaviors, trust, empathy, and love. It also regulates mood, reduces stress, and promotes sleep. | Positive social interactions, touch, experimental interventions |
| Cortisol | 5–25 mcg/dL (morning) | Produced by adrenal cortex; regulates stress response, metabolism, immune function | Stress management, regular sleep, moderate exercise |
| Insulin | 2–20 μIU/mL (fasting) | Secreted by pancreatic β-cells; promotes glucose uptake, regulates carbohydrate metabolism | Weight management, regular exercise, low-GI diet |
| Thyroid hormones (T4, T3) | T4: 5–12 μg/dL T3: 80–180 ng/dL | Produced by thyroid gland; regulate basal metabolic rate, brain development, mood | Adequate iodine intake, regular exercise, avoid goitrogens in excess |
| Estrogen (Estradiol) | Female: 30–400 pg/mL (varies by cycle) Male: 10–50 pg/mL | Produced by ovaries/testes; modulates mood, cognition, bone, and metabolic health | Weight-bearing exercise, healthy body weight |
| Testosterone | Male: 300–1000 ng/dL Female: 15–70 ng/dL | Produced by testes/ovaries; supports mood, cognition, muscle mass, metabolic health | Resistance training, adequate sleep, healthy fat intake |
| Leptin | Male: 0.5–6 ng/mL Female: 4–25 ng/mL | Secreted by adipocytes; regulates appetite, energy balance, and metabolism | Weight loss (if elevated), regular exercise, adequate sleep |
| Melatonin | Male: 18.3–134 pg/mL Female: 19.0–197 pg/mL Levels are significantly lower in the morning (8AM), reflecting the hormone’s circadian rhythm | Produced in the pineal gland, it acts as a free radical scavenger and protects cells from oxidative stress. It influences immune responses and may have anti-inflammatory effects. Melatonin helps synchronize various biological rhythms including and beyond sleep, like body temperature and hormone secretion. Emerging research points to potential roles in mood regulation and neuroprotection. | Maintain a regular sleep-wake schedule. Minimize exposure to artificial light, especially blue light, in the evening. Ensure exposure to natural daylight during the day. Practice good sleep hygiene in a cool, dark, quiet bedroom. |
Key physiologic pathways:
- Cortisol: Hypothalamic-pituitary-adrenal (HPA) axis; chronic elevation impairs mood and metabolism.
- Insulin: Pancreatic secretion in response to blood glucose; resistance leads to metabolic syndrome.
- Thyroid hormones: Hypothalamic-pituitary-thyroid axis; essential for neurodevelopment and metabolic rate.
- Estrogen/Oxytocin/Testosterone: Hypothalamic-pituitary-gonadal axis; influence mood, cognition, and metabolic health.
- Leptin: Adipose tissue to hypothalamus signaling; regulates satiety and energy expenditure
- Melatonin is produced in the pineal gland from the amino acid tryptophan, with synthesis and release tightly regulated by the light-dark cycle.
While melatonin is primarily produced in the pineal gland, it’s also made by our skin cells in response to sunlight, and it plays a hugely important role in skin health and metabolic regulation throughout the body. Melatonin acts on MT1 and MT2 receptors, which are widely distributed in the central nervous system. MT1 and MT2 receptors are also found in peripheral organs (e.g., blood vessels, GI tract, reproductive organs, immune system), where melatonin regulates physiological processes such as vascular tone, immune responses, and reproductive function.
Melatonin Pathways
| Pathway Type | Key Targets | Main Effects/Mechanisms |
| Membrane Receptors | MT1, MT2 (GPCRs) | ↓ cAMP, ↑ PLC/PKC, MAPK/ERK, PI3K/Akt, circadian effects |
| Intracellular | Quinone reductase 2, etc. | Antioxidant, cytoskeletal, redox modulation |
| Nuclear Receptors | Orphan nuclear receptors | Gene transcription regulation |
| Paracrine/Autocrine | Retinal cells | Enhances low-light retinal function |
Lifestyle interventions such as regular physical activity, stress reduction, adequate sleep, and balanced nutrition are central to optimizing the function of these hormones and supporting both mental and metabolic health.
BDNF & AMPK
There are two other pathways that are worth mentioning in a discussion of metabolic psychiatry.
- AMPK acts as a cellular energy sensor (“the master nutrient sensor”) and is a negative regulator of synaptic plasticity and memory formation in the hippocampus. High AMPK activity impairs memory and fear formation, likely through inhibition of mTORC1 and downstream effects on BDNF and synaptic proteins.
- BDNF is crucial for neuronal health, synaptic plasticity, and memory. Its expression is influenced by AMPK and mTORC1 signaling, and it is upregulated by interventions that promote neuroplasticity. BDNF can be upregulated by increasing your consumption of healthy foods containing Omega-3 fatty acids (flaxseeds, chia seeds, walnuts, fish oil), polyphenols (berries, grapes, vegetables, nuts), prebiotic fiber (bananas, oats, onions), and reducing your sugar and processed food intake. Getting 7-9 hours of sleep will increase BDNF. Photobiomodulation increases BDNF.
- Pharmacologic interventions that activate AMPK (e.g., metformin) are used for metabolic health, while antidepressants and experimental BDNF agonists may enhance BDNF signaling.
- Lifestyle interventions such as exercise, caloric restriction, and cognitive engagement optimize both AMPK and BDNF function, supporting both mental and metabolic health.
- Timing is important for AMPK activation: while AMPK directly acts to protect metabolic and mitochondrial health, Interventions that increase AMPK can blunt the positive effects of exercise like post-exercise muscle hypertrophy and post-exercise mitochrondrial adaptation, so hormetic interventions like intermittent fasting and metformin should be timed to avoid coinciding with post-exercise recovery. After you exercise, get some protein, and avoid metformin in recovery (metformin’s peak concentration is 3hrs after ingestion, half life 6hrs).
| Molecule/Pathway | Main Functions in Mental Health | Main Functions in Metabolic Health | Pharmacologic Interventions | Lifestyle Interventions |
| AMPK (AMP-activated protein kinase) | Negative regulator of synaptic plasticity and fear memory formation; high AMPK activity in the hippocampus impairs long-term memory and plasticity | Master cellular energy sensor; maintains energy homeostasis by activating catabolic pathways and inhibiting anabolic pathways when cellular energy is low | Metformin (activates AMPK), AICAR (AMPK activator) | Caloric restriction, intermittent fasting, regular physical exercise |
| BDNF (Brain-derived neurotrophic factor) | Promotes synaptic plasticity, learning, memory, and neuronal survival; essential for long-term memory formation] | Supports neuronal metabolism and energy balance; may influence appetite and glucose metabolism | Antidepressants and exercise increase endogenous BDNF but are not direct agonists. | Aerobic exercise, cognitive stimulation, adequate sleep, balanced diet |
Benefits correlated with higher BDNF levels
- Improved memory and learning: Elevated BDNF is associated with better memory retention and learning capacity.
- Mood regulation and well-being: Higher BDNF levels are linked to improved mood and emotional regulation, potentially reducing the risk of mood disorders.
- Cognitive preservation in aging: Increased BDNF helps maintain cognitive function and may protect against age-related cognitive decline and neurodegenerative diseases.
- Enhanced neuroplasticity: Higher BDNF supports the brain’s ability to adapt and reorganize in response to new experiences, injury, or disease.
Sleep quality and duration have a significant and scientifically validated effect on BDNF levels, with chronic sleep loss and insomnia lowering BDNF, and acute sleep deprivation sometimes causing a transient increase. Evidence suggests a role for specific nutrients like Omega-3s and polyphenols and dietary patterns like the Mediterranean diet in increasing BDNF levels. This jives with what we already know, that the Mediterranean diet offers significant benefits for cognitive function and brain morphology.
| PBM Wavelength | Evidence for BDNF Increase | Notes |
|---|---|---|
| 660 nm (red) | Yes | Red light therapy more than doubled BDNF levels via ERK/CREB pathway in hippocampal cells. |
| 808 nm (NIR) | Yes | NIR therapy more than doubled BDNF levels and improved cognitive function, with the effects persisting at follow-up 3 months after the intervention. |
Emerging research demonstrates that red and near-infrared light therapies are powerful tools in increasing BDNF expression.
Mitochondria and Oxidative Stress
How “Antidepressants” Work
The term “antidepressants” refers broadly to medications that improve symptoms of depression, anxiety, and related mood disorders. Their effects extend far beyond symptom relief, and even though they are called “antidepressants,” they’re even better at treating anxiety. Modern neuroscience shows that these medications don’t just alter brain chemistry — they help the brain heal, adapt, and rewire itself.
Antidepressants restore neurotransmitter balance, enhance neuroplasticity, and recalibrate brain circuits.
- SSRIs: Increase synaptic serotonin.
- SNRIs: Increase serotonin and norepinephrine.
- NDRIs: Increase dopamine and norepinephrine.
- MAOIs/TCAs: Rarely used but effective for treatment-resistant or atypical depression.
- Rapid-acting agents: Ketamine/esketamine modulate glutamate and BDNF pathways for fast symptom relief.
Neuroplasticity Effects:
- Receptor down/upregulation restores equilibrium.
- BDNF and synaptogenesis are upregulated, enhancing connectivity in prefrontal cortex, hippocampus, and amygdala.
- Adaptive changes can persist after medication discontinuation, provided adequate dose and duration.
By increasing the availability of these neurotransmitters, antidepressants help restore balance in brain circuits that have become dysregulated in depression and anxiety.
Neuroplasticity: Helping the Brain Rebuild Itself
One of the most profound effects of antidepressants is their ability to enhance neuroplasticity — the brain’s capacity to form new neural connections and reorganize itself.
This process underlies learning, memory, and emotional regulation.
When neurotransmitter levels are modulated by antidepressants, a cascade of downstream effects occurs:
- Receptor sensitivity adjusts: Certain receptor subtypes become less reactive (downregulated) to prevent overstimulation, while others are upregulated to restore equilibrium.
- Gene expression changes: Antidepressants influence genes that control the production of growth factors like BDNF (Brain-Derived Neurotrophic Factor), which supports neuron survival and synaptic growth.
- Circuit remodeling: Over time, these molecular changes enhance synaptic connectivity in key mood-regulating areas of the brain such as the prefrontal cortex, amygdala, and hippocampus.
The end result is greater emotional resilience and more stable mood regulation. Interestingly, these adaptive brain changes can persist long after the medication is discontinued — but only if the medication is taken at an adequate dose and for a sufficient duration to allow neuroplastic remodeling to occur.
Pleiotropic (System-Wide) Effects
Antidepressants have some pleiotropic effects, meaning they influence multiple biological systems beyond the brain:
- Cardiovascular benefits: SSRIs have been shown to improve outcomes in patients with heart disease, possibly by reducing platelet aggregation and inflammatory activation.
- Pain modulation: SNRIs can reduce chronic pain syndromes such as neuropathic pain and fibromyalgia by enhancing descending inhibitory pain pathways.
- Neurohormonal and immune modulation: Antidepressants can normalize stress hormone signaling (HPA axis) and temper pro-inflammatory cytokine activity.
- Cognitive and motivational enhancement: Bupropion’s dopaminergic activity may improve attention, focus, and motivation. Bupropion can also improve sexual dysfunction, and overweight or obese people on bupropion can experience 5-10% weight loss.
- Metabolic benefits: Bupropion is associated with modest weight loss (typically 5–10% in overweight patients) and may counteract SSRI-related weight gain.
- Vasomotor stability: SNRIs such as venlafaxine can reduce the frequency and intensity of hot flashes in peri- and postmenopausal individuals.
Antidepressants do not simply “boost serotonin.” They initiate a complex process of neural recalibration — restoring balance across multiple neurotransmitter systems, enhancing neuroplasticity, and improving overall physiological resilience. When taken correctly and consistently, they can help the brain regain its natural capacity for flexibility, stability, and well-being.
Mitochondrial Health
Mitochondria, the “powerhouses” of your cells, produce ATP—the energy your body and brain need for thinking, moving, repairing tissues, and regulating metabolism. They also help control inflammation, support cell survival, and influence how neurons communicate, making them vital for brain function, mood, and stress resilience.
- Exercise: High-intensity and resistance training stimulate mitochondrial growth in muscles and brain.
- Nutrition & Supplements: Omega-3s, CoQ10, alpha-lipoic acid, and creatine protect mitochondria, reduce oxidative stress, and support energy production.
- Pharmacologic/Nutraceutical Support: medications like telmisartan act on PPARγ to increase mitochondrial biogenesis and function.
- Red/Near-Infrared Light (Photobiomodulation): These therapies stimulate cytochrome c oxidase in mitochondria, increasing ATP production, reducing oxidative stress, promoting new mitochondria, and supporting cellular repair and neurotrophic signaling.
- By combining these strategies, you can optimize cellular energy, protect neurons, and improve overall resilience and health.
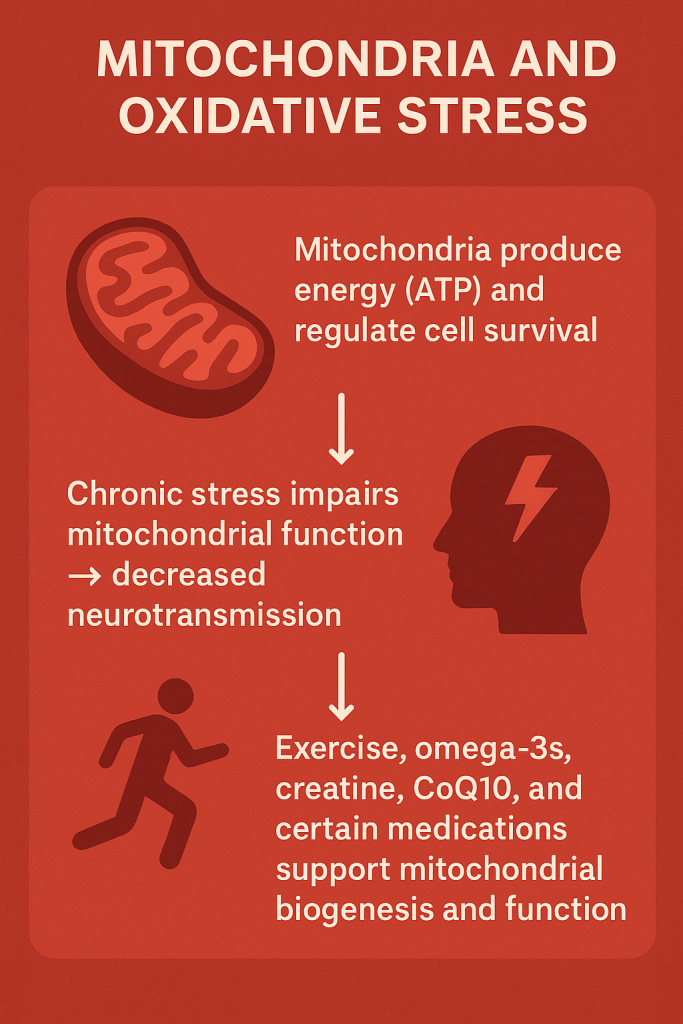
Chronic stress, poor diet, sleep loss, and toxins can impair mitochondrial function, leading to lower energy, increased free radicals, reduced neurotransmission, fatigue, brain fog, and mood disturbances.
Mitochondria are critical for brain signaling because neurons require large amounts of energy to communicate. When mitochondrial function is impaired, neurotransmitter production and synaptic activity can decline, contributing to anxiety, depression, and cognitive fog. Supporting mitochondria with exercise, omega-3s, CoQ10, and even red/NIR light therapy has been shown to improve both energy and mental well-being.
Photobiomodulation for your brain
PBM (specifically red light & near infrared light therapy) is a safe and effective way to improve brain metabolism, inflammation, anxiety, and depression, improve cognitive performance and reduce PTSD symptoms following traumatic brain injury, treat neurodegenerative diseases including multiple sclerosis. PBM reduces neuroinflammatory cytokines (TNF-α, IL-1β, and others), and it increases the expression of neurotrophic factors important for neuroplasticity. You can maximize the benefits of red & NIR light with a special device, but you can also get it by walking outside and getting some sunlight on your skin.
Alex Fergus measured the NIR/red light output from the sun (in Dubai and New Zealand) and gathered the following data:
| Time | Solar Red Light Output (620–680 nm) | Solar Near-Infrared Output (800–870 nm) |
|---|---|---|
| 6:30 am | 2.8 mW/cm² | 3.0 mW/cm² |
| 7:00 am | 4.8 mW/cm² | 4.8 mW/cm² |
| Midday | 8.7 mW/cm² | 8.0 mW/cm² |

Using today’s LED panels, you can maximize the benefits of near infrared & red light.
If you can catch the sun every morning, you can enjoy some of the benefits of NIR/red light therapy, but keep in mind that the irradiance of a dedicated NIR/red light panel or bulb will be much more powerful (typically 30-60 mW/cm²).
If you’re interested in learning more about PBM, read the HHNY PBM page.
Remember that lifestyle interventions provide us with immensely powerful mechanisms through which we can improve our mental and physical health.
Visit the lifestyle and longevity page to learn more about the Mediterranean diet, sleep, and exercise.
Visit the photobiomodulation page to learn more about red & near-infrared light therapy.
Visit the supplements page to learn about creatine and other supplements that can improve brain function and mental health.
