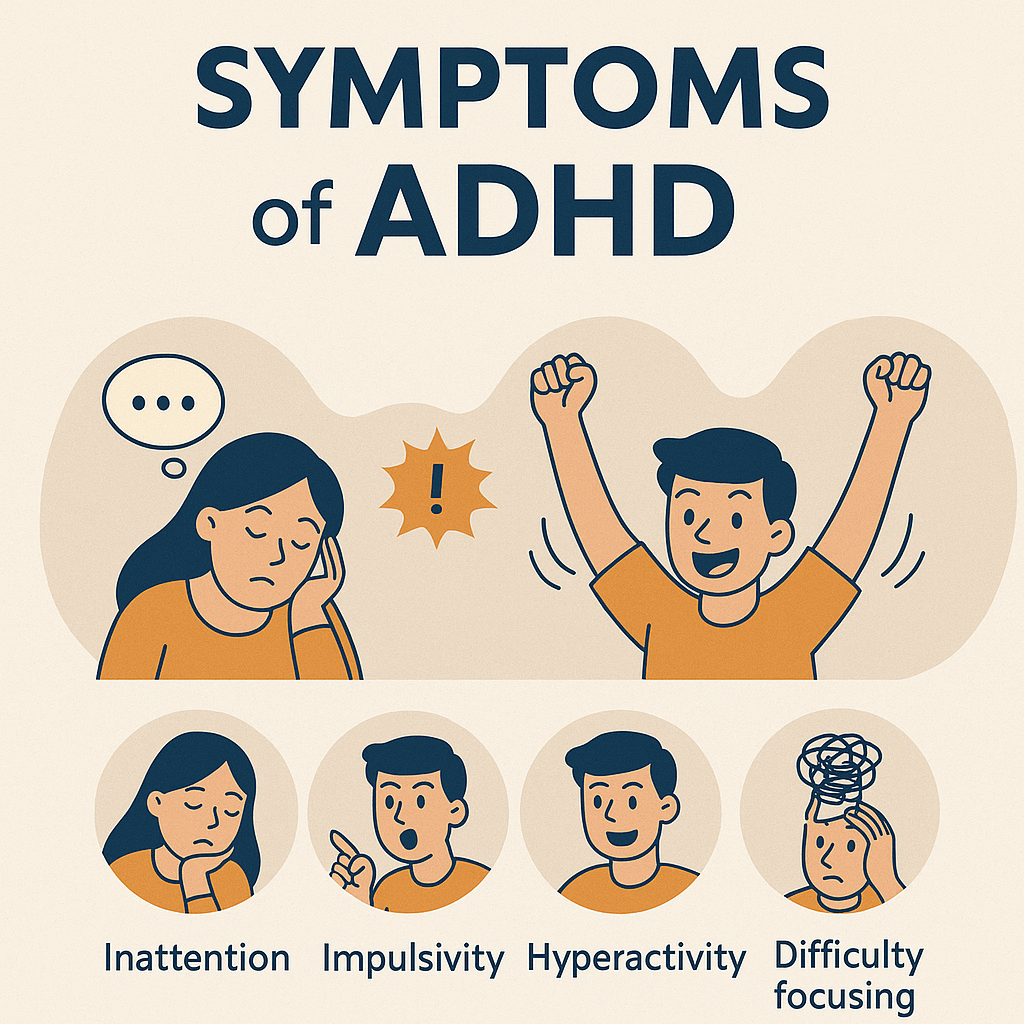
Understanding ADHD
Attention-Deficit/Hyperactivity Disorder (ADHD) is a common condition that affects children, teens, and adults. It can look very different from one person to the next, which is why ADHD is sometimes misunderstood or missed altogether. On this page we’ll discuss the features, diagnosis, treatment, and prognosis for people with ADHD.
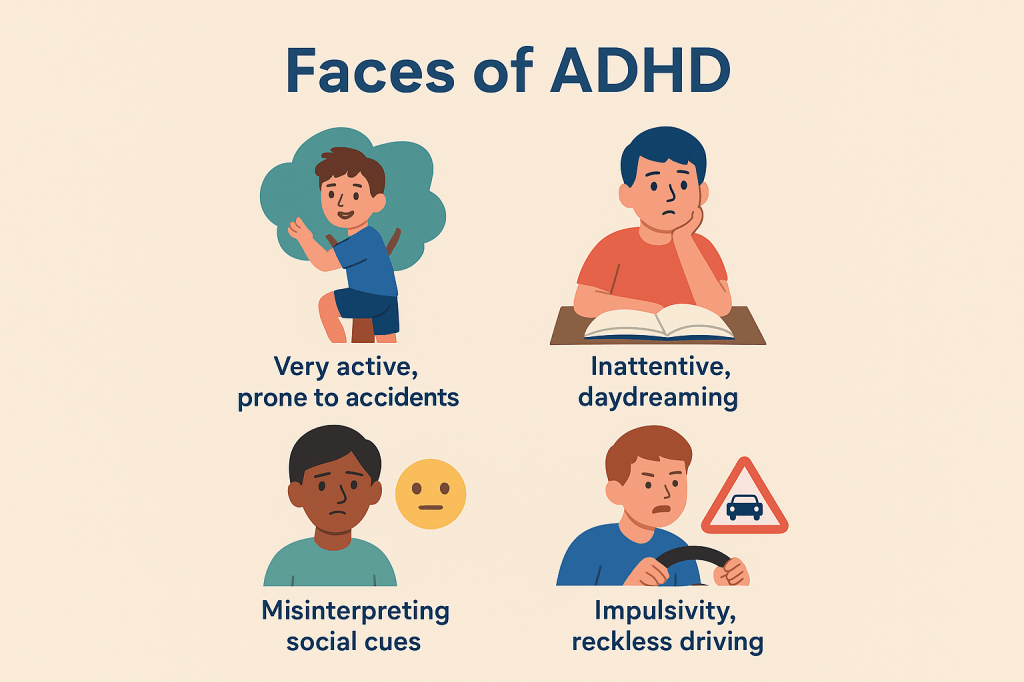
The Many Faces of ADHD
ADHD manifests differently in different people.
ADHD doesn’t look the same in every child or adult. Here are some common ways it shows up:
- The very active child – always on the move, prone to accidents, climbing, breaking things, diving into bushes. They may seem fearless, but they’re really struggling with hyperactivity and impulsivity.
- The inattentive student – daydreaming in class, struggling to finish work, and sometimes feeling “not smart,” even though their brain just works differently.
- The signal misreader – children or adults may interpret neutral social cues as negative because they’re used to being corrected or feel “on guard.”
- The impulsive person – risky driving, accepting dares, or experimenting with substances.
Diagnostic Challenges
Sometimes there’s more to the picture than ADHD.
ADHD is not always easy to diagnose because many other conditions can mimic it. For example:
- Anxiety, depression, or trauma may look like inattention.
- Learning difficulties (like dyslexia or math challenges) can be mistaken for ADHD.
- In teens, bipolar disorder or substance use may overlap with ADHD symptoms.
Clear cases of ADHD usually improve a lot with treatment—but that’s why careful assessment is so important.

Common Overlaps
ADHD often co-occurs with other conditions (called comorbidities):
- Learning disorders – trouble with reading, writing, or math.
- Mood disorders – depression or anxiety from years of negative feedback.
- Behavioral challenges – impulsivity sometimes looks like conduct problems.
- Autism, PTSD, head injury, or even post-COVID brain fog can share ADHD-like symptoms.
The Assessment
I use a combination of tools to evaluate ADHD:
- History – family background, medical issues, developmental milestones.
- Physical exam – including vitals, growth, and sleep/nutrition review.
- Collateral info – teacher feedback, home observations, school reports.
- Testing – rating scales and sometimes computerized attention tests.
Pharmacotherapy
Read about pharmacotherapeutic interventions for ADHD
Treatment is individualized and may include:
Stimulant medications
- Methylphenidate (often fewer side effects in kids)
- Dextroamphetamine (stronger, requires careful dosing)
- Lisdexamfetamine (similar to DXA, also approved for binge-eating disorder)
- Bupropion (not as strong as amphetamines, but may be helpful for people who are also depressed, trying to quit smoking, or get anxious on stronger stimulants)
Non-stimulants
- Guanfacine, clonidine (calming, sometimes help with sleep)
- Atomoxetine, viloxazine (SNRI-like, different side effect profile, may also be helpful with symptoms of depression)
Non-drug Interventions
Improve ADHD symptoms using these strategies in conjunction with medication or instead of medication.
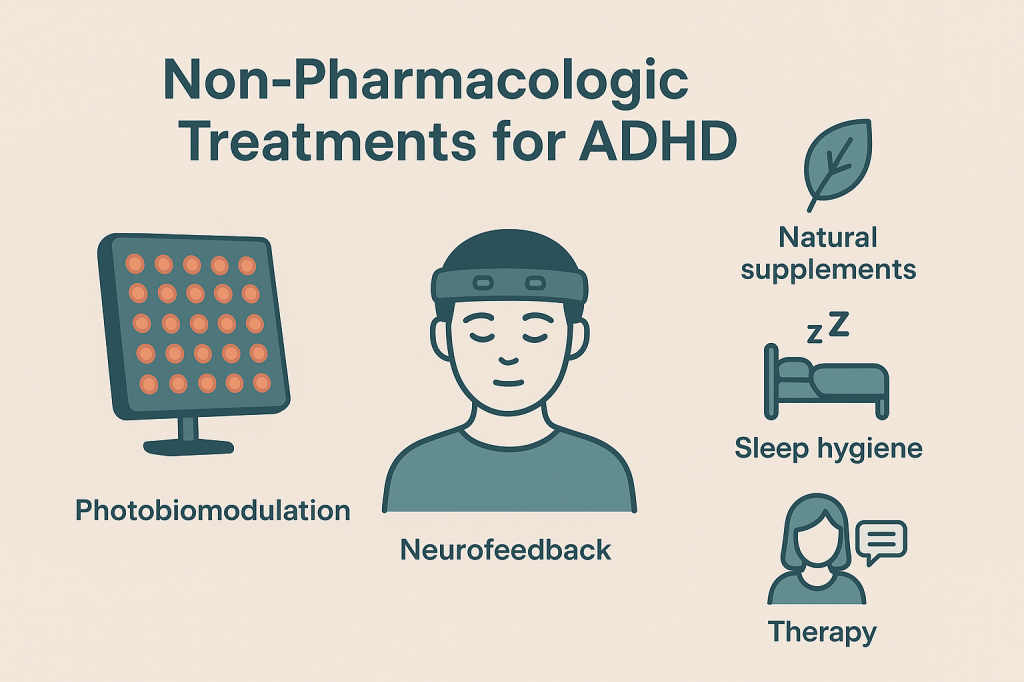
- Cognitive behavioral therapy and parent training.
- Discovering your learning style and catering to it w/ school accommodations and learning supports: improves functional outcomes and academic performance.
- Utilizing experiential learning rather than traditional didactic styles.
- Getting between 7-9 hours of good sleep every night, and bright light therapy for correction of circadian delay may improve symptoms of ADHD.
- NIR/red light therapy can improve attention in ADHD, and high-frequency pulsed-NIR brainwave entrainment has the potential to counteract theta/delta wave predominance seen in people with ADHD, OCD, and schizophrenia.
- Meditation with neurofeedback are emerging as highly personalized interventions to approve attention. Similarly to brainwave entrainment strategies, people can use a device like the Muse EEG headband (Muse S Athena $475 | Muse 2 [used] ~$200) to improve attention and response inhibition by suppressing theta waves and enhancing beta waves. Alpha wave enhancement may also have some benefit for working memory in ADHD.
- Omega 3 supplementation can offer a modest reduction in ADHD symptoms, and it’s a safe adjunctive therapy with mood and cardiovascular benefits as well.
- Eating a Mediterranean diet lowers the incidence of ADHD
- Vitamin D3 supplementation have been shown to improve ADHD in the setting of deficiency (which is common).
- Low magnesium levels are correlated with increased incidence of ADHD, and this trial found that supplementation resulted in decreased coduct and social problems in ADHD
- Creatine supplementation can improve cognitive/executive functioning, memory, and many of the symptoms that are associated with ADHD. Higher doses of creatine are necessary for brain penetration.
- Lactobacillus rhamnosus probiotics: early studies suggest possible benefit
Prognosis
What to expect from treatment
ADHD is common—affecting about 5–10% of people worldwide—and it often continues into adulthood. With proper diagnosis and treatment, people with ADHD experience:
- Better health
- Stronger school or work performance
- Improved relationships
- A longer and higher-quality life
Attention-deficit/hyperactivity disorder is considered straightforward to treat with stimulant medications because these medications have very high efficacy, rapid onset of action, and a favorable safety profile in the majority of pediatric and adolescent patients.
ADHD medications have perhaps the largest effect size of all psychiatric medications, and people tend to see a rapid improvement with treatment.
ADHD is considered a variety of neurodiversity—a different but valuable way of thinking. With understanding, support, and the right treatment, ADHD can be managed, and strengths can shine.
The most robust longitudinal studies indicate that approximately 20–30% of childhood attention-deficit/hyperactivity disorder (ADHD) resolves with age, meaning these individuals no longer meet full diagnostic criteria for ADHD by adulthood. Many children with ADHD find that their symptoms improve in their late teens or 20s as their prefrontal cortex develops.
It is worth considering that even people with considerable symptom burden from ADHD do not need to function at peak performance at all times. Children and adults might find they can take a holiday from the medication during the weekends. Adults in retirement age might find that they don’t really need to take medication at all any longer because their lives have become less demanding.
